Imagine an army of self-propelling, radioisotope-covered particles 2500 to 10,000 times smaller than a speck of dust that, upon injection into the body, search for and attach themselves to cancerous tumours, destroying them. Sounds like science fiction? Not so for mice with bladder cancer.
Researchers in Spain report that nanoparticles containing radioactive iodine and which propel themselves upon reaction with urea have the ability to distinguish cancerous bladder tumours from healthy tissue. These “nanobots” penetrate the tumour’s extracellular matrix and accumulate within it, enabling the radionuclide therapy to reach its precise target. In a study conducted at the Institute for Bioengineering of Catalonia (IBEC) in Barcelona, mice receiving a single dose of this treatment had a 90% reduction in the size of bladder tumours compared with untreated animals.
This novel approach may one day revolutionize the treatment of bladder cancer. Bladder cancer is the tenth most common cancer in the world, with over 600,000 new cases diagnosed in 2022 and more than 220,000 deaths globally, according to the World Health Organization’s Global Cancer Observatory.
Non-muscle-invasive bladder cancer, which accounts for 75% of cases, is currently treated by tumour resection followed by intravesical injection of chemotherapy or immunotherapy drugs into the bladder. Drug delivery is particularly challenging, however, due to the low permeability of the urothelium (the tissue lining the inside of the urinary tract), content filling of urine and subsequent washout of drugs. The process is also uncomfortable for patients, as they need to turn their bodies at intervals while lying prone to enable the drugs to reach all sides of the bladder wall. Following treatment, there’s a 30–70% risk of recurrence within five years.
To improve clinical outcomes, principal investigator Samuel Sánchez and colleagues aim to develop innovative and more effective bladder cancer treatments, and in the process, reduce recurrence rates. Additionally, a single-dose therapy would significantly reduce the cost of treatment, which currently requires between six and 14 hospitalizations.
The team created nanobots from mesoporous silica nanoparticles with various functional components on their surfaces. These include radioisotopes for PET visualization or radionuclide therapy, and the protein urease, which reacts with urea in urine and enables the nanobot’s propulsion.
Writing in Nature Nanotechnology, the researchers report that when they added a droplet of nanobots to a solution containing 300 mM urea, the nanobots exhibited a swarming motion, forming active and vigorous fronts and three-dimensional vortices. Without the urea, the nanobots simply sedimented near the addition site.
To examine whether the nanobots can reach a tumour in vivo, the team assessed their behaviour in tumour-bearing mice. Positron emission tomography (PET) images showed that signals from radiolabelled nanobots were co-located with the tumour position, as determined via MRI, with radioactivity primarily seen at the target tumour site. Only mice injected with nanobots plus urea showed substantial accumulation in the tumour mass – nanobots delivered in water, and control nanoparticles (without urease) delivered in water or urea exhibited minimal tumour uptake.
The researchers suggest that the mobility of the nanobots helps them to penetrate the tumour mass. “Nanobots lack specific antibodies to recognise the tumour, and tumour tissue is typically stiffer than healthy tissue, but this is not the case in bladder tumours” explains co-first author Meritxell Serra Casablancas of IBEC. “We observed that these nanorobots can break down the extracellular matrix of the tumour by locally increasing the pH through a self-propelling chemical reaction. This phenomenon favoured greater tumour penetration.” The researchers believe that the nanobots collide with the urothelium as if it were a wall, but penetrate the tumour which is spongier.
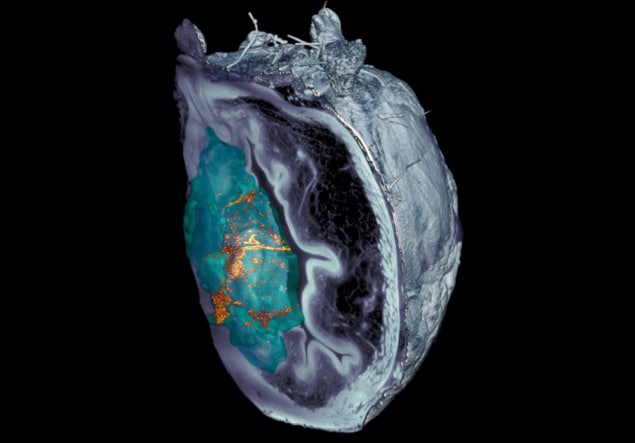
The team note that identifying the nanobots in microscopy images of dissected tissue was challenging. After confocal optical microscopy techniques failed, researchers at IRB Barcelona developed a light-sheet-based microscopy system, based on planar laser illumination, capable of scanning the different layers of the bladder and creating a 3D reconstruction of the entire organ.
“The scattered elastic light-sheet microscopy system that we developed enabled us to eliminate the light reflected by the tumour itself, allowing us to identify and locate nanoparticles throughout the organ without prior labelling, at unprecedented resolution,” says Julien Colombelli from IRB Barcelona.

Engineered bacteria attract cancer-killing radioisotopes into tumours
To evaluate the technique’s therapeutic effect, the team labelled nanobots with the iodine-131 (131I, a radioisotope commonly used for radionuclide therapy), and administered them to the tumour-bearing mice. Treatment with lose-dose 131I-nanobots in urea arrested tumour growth, while high-dose 131I-nanobots administered in urea led to a nearly 90% reduction in tumour volume compared with non-treated animals.
Sánchez tells Physics World that the team’s next steps are to encapsulate small drugs currently used in chemotherapy and continue to test the efficiency of nanobots as drug carriers. They eventually intend to scale up the nanobots and study the regulatory pathways to move towards the first clinical trials in the next three to four years, via the IBEC spinoff Nanobots Therapeutics.