Epilepsy is one of the most common neurological disorders. While many patients can control epileptic seizures using drugs, almost one-third don’t respond to medication. Patients with such drug-resistant epilepsy are instead treated by removing the brain regions from which seizures originate. Before such surgery, however, it’s essential to identify these epileptogenic zones with extreme precision.
To maximize the success of epilepsy surgeries, researchers from the Institut de Neurosciences des Systèmes (INS) at Aix-Marseille Université have developed the virtual epileptic patient (VEP), a digital workflow for estimating a patient’s epileptogenic zone networks (EZNs) based on MR imaging and electrical activity recordings.
“There is a clinical need for this: surgery success rate in epilepsy has not significantly improved in the past 40 years,” says lead author Viktor Jirsa, INS director and a lead scientist in the Human Brain Project and The Virtual Brain.
“Epilepsy is a network disease and it is thus perfectly suited to be addressed by a network approach as we have developed in The Virtual Brain,” Jirsa explains. “In the Human Brain Project, we have developed the methods to personalize brain networks, thus clinical applications using digital twins for network disorders are the next natural step.”
The VEP, described in Science Translational Medicine, works by constructing a whole-brain model personalized for each particular patient. The model comprises a network of regions, each representing a node in the brain network. It uses the patient’s anatomical T1-weighted MRI data to define the structural scaffold of the brain and diffusion-weighted MRI to estimate connection strengths between brain regions – creating a patient-specific structural connectivity matrix.
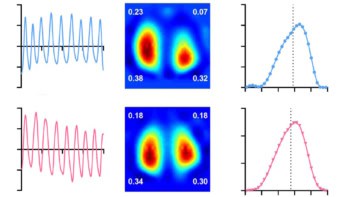
The neural dynamics of each network node are defined using a neural mass model, a set of equations that represent the dynamics in that brain region. To estimate the locations of the EZNs, the model uses data from the patient’s stereo-electroencephalography (SEEG) recordings, along with CT scans to localize the implanted SEEG electrodes, to simulate the spread of abnormal activity during epileptic seizures.
Assessing patient data
After validating the model using synthetic data, Jirsa and colleagues applied the VEP workflow to data from a 29-year-old female patient with left frontal epilepsy. Using SEEG recordings from four of the patient’s seizures, the VEP identified three brain regions as EZNs, two of which had also been identified by clinicians based on SEEG signal analysis.
The patient had undergone surgical resection of the clinically defined EZNs. This reduced her seizure frequency but a couple of weeks later, the seizures returned. “Five months ago, she underwent surgery again, removing also the third EZN identified by VEP,” Jirsa tells Physics World. “Since then, she is seizure free.”

In addition to EZN estimation, the personalized brain models can also be used to predict the outcomes of different surgical interventions – a process referred to as “virtual surgery”. This could be used, for example, to determine the minimum number of brain regions that can be treated to provide seizure control while optimizing functional outcome.
For the abovementioned patient, the team used VEP simulations to predict the outcome of two virtual surgery schemes: removing the two brain regions identified by the clinicians; and removing the brain regions as performed in her actual surgery. Both virtual surgeries predicted seizure reduction but not elimination, consistent with the actual post-surgical outcome, reinforcing the potential clinical relevance of the VEP toolset.
To further evaluate the performance of the VEP workflow, the researchers retrospectively assessed the predicted EZNs for 53 patients with drug-resistant focal epilepsy. The VEPs reproduced the clinically defined EZNs (based on pre-surgical assessments) with a mean precision of 0.613 and a small mean physical distance (5.6 mm) between VEP-identified and clinically defined epileptogenic regions.
They also examined the VEP’s false discovery rate (FDR) in 25 patients who underwent epilepsy surgery. For those who were seizure-free following resection, the VEP showed a small mean FDR of 0.028. With these seizure-free patients, it is likely that the EZN was completely removed and that thus a false-positive estimate most likely falls outside the EZN.

Treating epilepsy with physics
In patients who were not seizure-free after treatment, a false-positive estimate has a high possibility of corresponding to non-resected epileptogenic regions. In this group, the VEP results had a larger mean FDR of 0.407, suggesting that it may be possible to exploit the predictive power of the VEP to improve surgical planning.
The researchers conclude that this personalized whole-brain network modelling could play an important role in both diagnostics and treatment of patients with drug-resistant epilepsy. “We are currently working on virtual surgery approaches optimizing surgical effectiveness, as well as non-invasive stimulation for diagnostic and therapeutic purposes,” says Jirsa.
The VEP is now being evaluated prospectively in an ongoing clinical trial (EPINOV) recruiting 356 patients from 11 epilepsy centres in France.