Degenerative diseases of the retina can damage or destroy photoreceptor cells, resulting in severe vision impairment. One promising way to restore lost vision is to implant an electronic retinal prosthesis, which works by detecting external light and stimulating inner retinal neurons such as ganglion and bipolar cells in response.
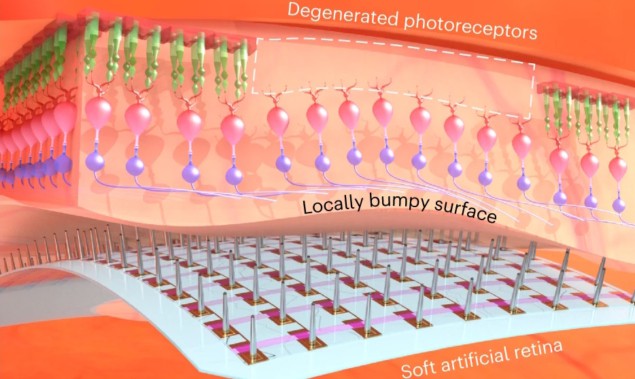
Existing retinal implants, however, contain rigid stimulation electrodes that could damage soft retinal tissue. They also suffer from a mismatch between the rigid electrodes and the curved retinal surface, which can be particularly irregular in patients with severe retinal degenerative disease.
To address these limitations, a research team headed up at Yonsei University in Korea has developed a soft retinal prosthesis that combines flexible ultrathin phototransistor arrays with stimulation electrodes made from eutectic gallium–indium alloy, an intrinsically soft liquid metal with low toxicity.
To create this “artificial retina”, first author Won Gi Chung and colleagues started with a high-resolution phototransistor array (50 × 50 pixels with 100 µm pitch) and 3D printed liquid metal electrodes on top. The electrodes form an array of pillar-like probes (20 µm in diameter and 60 µm in height) that, when placed on the retinal surface, directly stimulate retinal ganglion cells (RGCs).
The tip of each electrode is coated with platinum nanoclusters, which add nanometre-scale roughness and improve charge injection into the retinal neurons. Illuminating the phototransistors generates a photocurrent that injects charge into the RGCs through the electrodes. The action potentials evoked within the RGCs then travel to the optic nerve to create the visual information.

The researchers performed various in vivo tests to assess the biocompatibility of the device. Five weeks after implantation into live retinal degenerative (rd1) mice, they found no signs of bleeding, inflammation or cataracts and no significant impact on retinal thickness. They note that the device’s epiretinal placement – inside the vitreous with the electrode tips positioned on the RGC layer – is safer and less invasive than the subretinal implantation required by previous implants.
To evaluate their artificial retina further, the team performed ex vivo experiments by placing the device on isolated retinas from both wild-type and rd1 mice. Visual stimulation with blue light (performed without device operation) induced a response in the wild-type retina but not the rd1 retina. Electrical stimulation during device operation caused RGC spikes in both retinas, with a similar magnitude of electrically evoked potential in the wild-type and rd1 retinas.
In vivo vision restoration
Next, the team examined whether the device could restore vision to rd1 mice with a fully degenerated photoreceptor layer. Attaching the device to the animal’s retinal surface caused no notable damage or bleeding, and the electrodes remained intact when implanted onto the retinal surface.
The researchers then projected visible light onto the animal’s eye and recorded the real-time neural responses on the retina. Due to the complexity of retinal activity, they used unsupervised machine learning for signal processing. They found that the illumination induced spiking activity in the RGCs of the animal’s retina, creating RGC spikes with consistent potential magnitude and firing rates.
To investigate whether the implant can be used for object recognition, the researchers also exposed the eye to laser light through a patterned mask, observing that illuminated areas exhibited larger retinal responses than areas remaining in the dark. Comparing the maximum firing rates recorded from fully illuminated electrodes and dark-state electrodes showed that the RGC activity in the illuminated areas was about four times higher than the background RGC activity.

Ultrasound beams activate neurons in the eye to help restore vision
“The in vivo experiments confirmed that the signal amplification due to visible-light illumination induces real-time responses in the RGCs of the local area where the light is incident for live rd1 mice with massive photoreceptor degeneration, suggesting the restoration of their vision,” the researchers write. They point out that these findings could be used to help develop personalized artificial retinas for patients with uneven retinal degeneration.
Next, the team plans to conduct examinations of the artificial retina on larger animals. “After thoroughly validating our device on larger animals, our ultimate goal is to conduct clinical trials,” Chung tells Physics World.
The researchers report their findings in Nature Nanotechnology.



